Trichomoniasis is a common sexually transmitted infection. It affects an estimated 3.7 million people in the United States yearly. This infection can be serious, especially for pregnant women. Knowing about the symptoms, causes, and treatments is important.
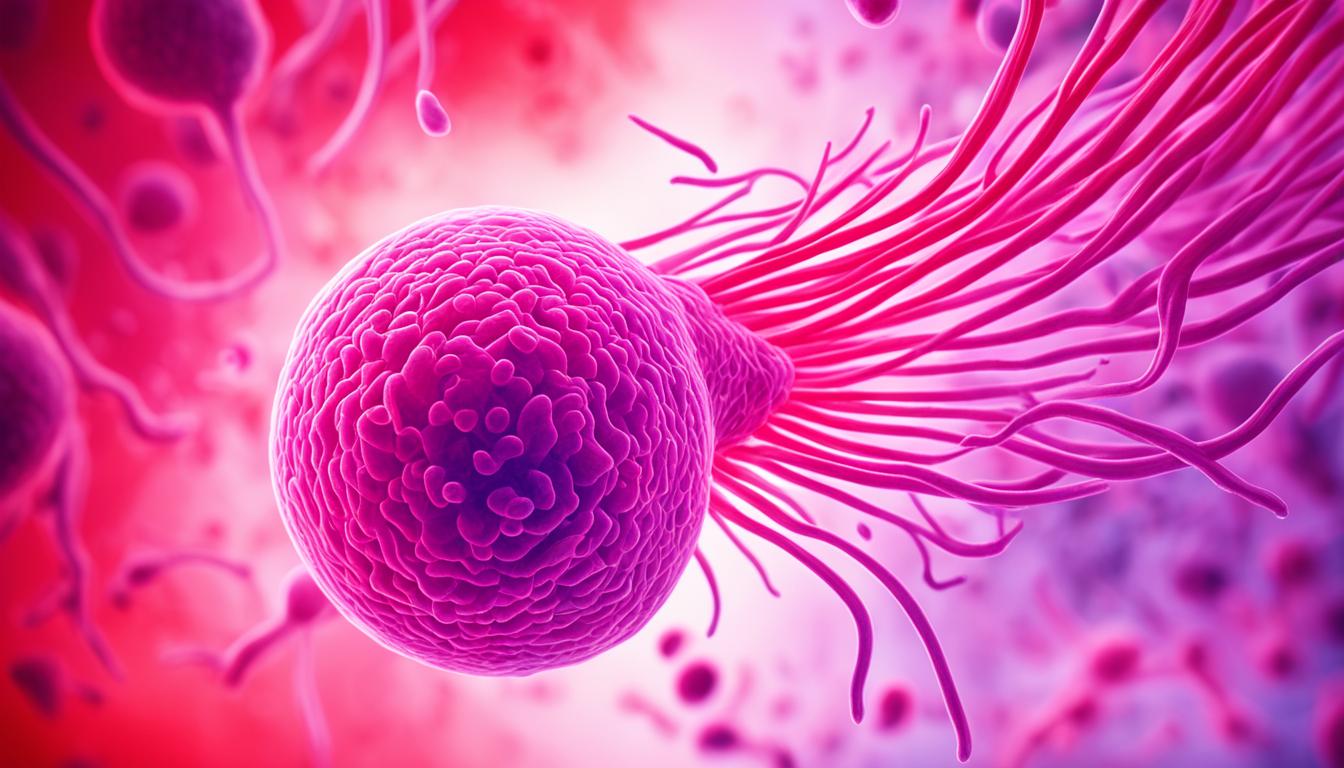
It’s caused by a parasite called Trichomonas vaginalis. It affects the lower genital tract in both men and women. In women, it leads to vaginitis. This can cause foul-smelling discharge, itching, and painful urination. But, about 70% of those infected show no symptoms. This makes diagnosis and treatment hard, raising the risk of spreading the infection.
Good news is, trichomoniasis is curable. Antibiotics like metronidazole are used to treat it. It’s important for all sexual partners to get treated together to avoid reinfection. Practicing safer sex by using condoms and limiting partners is essential too. These steps can help lessen the risk of getting or spreading trichomoniasis.
Key Takeaways
- Trichomoniasis is a common sexually transmitted infection caused by the parasite Trichomonas vaginalis.
- In women, it can cause symptoms like foul-smelling discharge and itching. But about 70% of people don’t notice any symptoms.
- Treatment involves antibiotics. It’s vital for all partners to get treated to avoid spreading the infection again.
- Trichomoniasis can also increase the risk of other STIs. In pregnant women, it may lead to preterm delivery or low birth weight.
- Practicing safer sex, such as using condoms and having fewer partners, can prevent trichomoniasis.
What is Trichomoniasis?
Overview of the Sexually Transmitted Infection
Trichomoniasis is a common STI caused by a parasite named Trichomonas vaginalis. It’s among the top non-viral STIs in the U.S., affecting around 3.7 million people. The parasite infects the genital tract, targeting the vagina, cervix, and urethra in women. In men, it mostly goes for the urethra.
Causes and Risk Factors
This STI spreads mainly through sexual contact, which can be vaginal, oral, or anal sex. If you have many sexual partners or have had other STIs, you’re more at risk. Unprotected sex also increases your chances of getting trichomoniasis.
Trichomoniasis Symptoms
Trichomoniasis is a type of infection passed through sex. Both men and women can get it. However, the symptoms are not the same for everyone. Many people with it don’t show any signs. But for those who do, they might find the symptoms quite bothersome.
Signs and Symptoms in Women
Women might notice a bad, thin, greenish-yellow vaginal discharge with genital itching. They might also feel pain while peeing or having sex. Some could have a sore belly too. These symptoms usually show up within a month of getting the infection. But half of the women don’t feel anything.
Signs and Symptoms in Men
Men, on the other hand, are less likely to have symptoms. It’s about 30% of them. If they do, they might feel itchy inside the penis or have burning with urination. They could also see a thin, white discharge from the penis.
Not showing symptoms doesn’t mean it’s not there. This is why regular check-ups are so important. Finding and treating trichomoniasis early can stop it from spreading and causing troubles.
When to See a Doctor
If you have any symptoms of trichomoniasis like weird vaginal discharge or pain when you pee, see a doctor quickly. It’s also wise to visit your doctor who can check you, especially if you’ve been with someone diagnosed with trichomoniasis. Quick tests and treatment help stop spreading the infection and other problems.
| Symptom | Percentage of Affected Individuals |
|---|---|
| No symptoms (asymptomatic) | About 70% |
| Develop symptoms | Only about 30% |
| Recurrence within 3 months of treatment | Around 20% |
Trichomoniasis is tricky to find sometimes. Its signs are like those from other STIs. Special health centers may be better for checking if you have it. They can even send you to a specific clinic for more tests and care.
When your doctor suspects trichomoniasis, they may tell you to start treatment early. This is important as soon as the suspicion starts. After the test shows trichomoniasis, it’s key for your current partner and others you’ve been with to get checked and treated too. This step helps prevent getting the infection again.
Diagnosis and Testing
Healthcare providers might start by checking any signs of trichomoniasis during a physical exam. They may do a pelvic exam for women. This helps see if there’s an infection. They use Laboratory tests like checking vaginal or urethral fluids under a microscope. Or they use nucleic acid amplification tests (NAATs) to find the Trichomonas vaginalis parasite.
Physical Examination
During the physical exam, doctors search for signs that could mean trichomoniasis. They look for swelling or redness in the genital area. Women might also get a pelvic exam to check their vagina and cervix more closely.
Laboratory Tests
For a firm trichomoniasis diagnosis, lab tests on samples are needed. Doctors test these samples under a microscope. They might also use nucleic acid amplification tests (NAATs). These tests are the best way to find the Trichomonas vaginalis parasite.
Home Testing Options
Some people might be able to use at-home testing kits and then send the samples to a lab. However, these kits might not be easy to find everywhere. This approach means people can check for trichomoniasis without going to a clinic.
Complications of Untreated Trichomoniasis
Leaving trichomoniasis untreated can result in serious issues. For pregnant women, the risks are high. They might have their babies too early or with a low weight. This can lead to health and development problems for the child.
Risks During Pregnancy
Not treating Trichomonas vaginalis can lead to problems during pregnancy. Such issues include low birth weight, early birth, and early membrane rupture. Trichomoniasis can greatly affect the health of both the mother and her baby.
Increased Risk of Other STIs
Trichomoniasis also boosts chances of getting or spreading other STIs. This includes HIV, the virus that leads to AIDS. In places where both trichomoniasis and HIV are common, the risk of getting HIV can go up by 50%.
Also, trichomoniasis might up the risk of cervical and prostate cancer. Studies link T. vaginalis to cervical cancer and slightly higher PSA levels. PSA is a cancer marker, and its rise may hint at prostate complications.
Knowing about these risks is important. It highlights the need for getting tested and treated for trichomoniasis early. This can stop the infection from spreading and lower chances of severe health problems. Act quickly, and you can avoid many complications.
Trichomoniasis Treatment
The standard way to treat trichomoniasis is by taking antibiotics by mouth. Common ones are metronidazole (Flagyl), tinidazole (Tindamax), or secnidazole (Solosec). They can be given all at once or a bit each day for a few days. Make sure to take the full dose, even if you feel better before it’s done.
Antibiotic Medications
People with trichomoniasis often get metronidazole for 5 to 7 days. It’s known to work well. Yet, it might cause nausea, vomiting, or make things taste funny if you don’t eat first. Mixing it with alcohol is a bad idea and can cause strong reactions. Pregnant or breastfeeding moms should be careful with this medicine.
Partner Treatment
It’s also very important that your sexual partners get treated to avoid spreading the infection back to you. If symptoms don’t go away, checking for other diseases is wise. While being treated, avoid sex to stop passing it around again. Wait at least a week after antibiotics to make love safely.
Prevention Strategies
The best way to avoid trichomoniasis is by not engaging in sexual activities. If you are sexually active, using condoms every time you have sex can greatly lower the transmission of trichomoniasis. It is important to avoid douching since it can interfere with the natural bacteria balance in the vagina. This leads to a higher risk of infections like trichomoniasis. Also, having fewer sexual partners and getting tested regularly for STIs can help lessen the risk further.
Safer Sex Practices
Using condoms correctly each time you have sex, no matter if it’s vaginal, oral, or anal, is a key step to prevent trichomoniasis from spreading. Condoms act as a barrier, stopping the parasite from moving between partners.
Avoiding Douching
Douching alters the vaginal bacteria balance, making you more vulnerable to trichomoniasis and other vaginal infections. To decrease your chances of getting trichomoniasis, it’s best to steer clear of douching.
Limiting Sexual Partners
Having fewer sexual partners decreases your risk of getting trichomoniasis and other STIs. It’s crucial to get tested for STIs regularly, particularly if you have multiple partners or have had trichomoniasis before.
Trichomoniasis and Bacterial Vaginosis
Trichomoniasis and bacterial vaginosis are types of vaginitis. This means there’s an issue with the normal organisms in the vagina. They share some symptoms, like odd vaginal discharge. But they are caused by different things. Trichomoniasis comes from the parasite Trichomonas vaginalis. BV is due to too many specific bacteria. Since their causes are different, it’s vital for doctors to diagnose them correctly.
About 30% of those with trichomoniasis might feel symptoms. But about 70% don’t show any signs. On the other hand, most women with bacterial vaginosis won’t notice any symptoms. Trichomoniasis spreads through sex, but bacterial vaginosis doesn’t.
The way we treat these diseases is also distinct. Oral or vaginal medicines target bacterial vaginosis. For vaginal trichomoniasis, we often use antibiotics by mouth.
Recurrence and Retesting
After being treated for trichomoniasis, some may get it again. It affects about 20% of people within 3 months after treatment. If a sexual partner remains untreated, or if you’ve started sexual relationships with new partners, getting tested again is wise. When it’s time to retest, both partners should avoid sex for a week to 10 days.
| Metric | Value |
|---|---|
| Percentage of patients who may experience treatment failure leading to recurrent trichomoniasis | 2% to 5% |
| Percentage of women who report reinfection within 3 months of treatment | Up to 17% |
| Recommended treatment for women with recurrent trichomoniasis after a single-dose metronidazole | Metronidazole 500 mg twice daily for 7 days |
| Recommended treatment for resistant trichomoniasis | Tinidazole 2 to 3 g for 14 days |
If resistant trichomoniasis is suspected, it’s important to test for metronidazole and tinidazole effectiveness. Doctors might suggest other treatments, like the combination of paromomycin and tinidazole, for stubborn infections.
Trichomoniasis in Pregnancy
Exactly what might happen if a pregnant woman gets trichomoniasis? She and her baby could face some serious risks. This includes early birth and having a baby that’s too small. But this doesn’t have to be the end of the story. Luckily, we can fight trichomoniasis with the right medicines. Doctors and moms-to-be can work together on the best plan.
| Statistic | Value |
|---|---|
| Trichomoniasis affects approximately 2.6 million persons in the United States | 2.6 million |
| U.S. population-based T. vaginalis prevalence among females | 2.1% |
| U.S. population-based T. vaginalis prevalence among males | 0.5% |
| Highest trichomoniasis rates among Black females | 9.6% |
| Highest trichomoniasis rates among Black males | 3.6% |
| Trichomoniasis can cause a 1.4-times greater likelihood of preterm birth and other reproductive complications | 1.4-times |
Trichomoniasis is a big concern for pregnant women. It increases the chances of having the baby too early or very small. It can also make a mom-to-be more likely to get HIV during pregnancy. Trichomoniasis could lead to early birth, but not miscarriage. Treatment during pregnancy involves safe antibiotics.
Premature birth and low birth weight are two of the leading causes of death for babies.
In rare cases, babies can get trichomoniasis during birth. Most pregnant women won’t get checked unless they show signs like unusual discharge. Luckily, treating trichomoniasis during pregnancy is safe.
It’s best for both partners in a sexual relationship to avoid sex until they both finish treatment. Condoms can help lessen the chance of spreading trichomoniasis and other infections. Remember, trichomoniasis isn’t the only threat to pregnancy. Bacterial vaginosis and yeast infections can also cause problems.
Asymptomatic Trichomoniasis
Around 70% of people with trichomoniasis don’t show any symptoms. This is called asymptomatic trichomoniasis or trichomoniasis without symptoms. It means these people might not know they’re infected. They could pass the parasite to their partners without knowing. This silent spread can lead to more sexually transmitted infections.
If you have several partners or had trichomoniasis before, getting tested is crucial. Testing can catch asymptomatic trichomoniasis early. Then, steps can be taken to stop the parasite from spreading further. This also helps in avoiding the problems that come with untreated trichomoniasis.
Trichomoniasis in Non-Sexual Transmission
Trichomoniasis mainly spreads through sexual contact. Sometimes, it might spread in non-sexual ways, like sharing towels or using the same toilet seat. However, these ways are not fully proven.
This infection usually doesn’t spread by casual, non-sexual touch, including hugs or kisses. The non-sexual transmission of trichomoniasis is rare, with most cases linked to sex.
| Reported Cases of Non-Sexual Trichomoniasis Transmission |
|---|
|
Some cases point to the chance of non-sexual transmission of trichomoniasis. But we need more studies to know for sure how often this happens and how. Even so, it’s smart to be clean, not share personal stuff, and take care of your hygiene against trichomoniasis.
Living with Trichomoniasis
Being diagnosed with trichomoniasis is scary but treatable. After diagnosis, the key is getting proper antibiotic treatment. It’s important to finish the whole treatment. Plus, make sure your sexual partners are also tested.
This helps prevent you from getting the infection again. With this approach, you can manage trichomoniasis and reduce further risks.
Dealing with trichomoniasis can be tough. But, it’s common and can be treated. Seeking medical help and taking preventive steps are crucial. They help you regain control over your health.
Under the right guidance and with proper understanding, living with trichomoniasis gets easier.
Conclusion
Trichomoniasis is a common STI caused by the parasite Trichomonas vaginalis. It leads to symptoms like strange vaginal discharge, genital irritation, and pain when peeing. But, many people with trichomoniasis don’t show any symptoms.
Getting tested and treated quickly is key. This helps prevent other STIs and issues during pregnancy. Using condoms, staying monogamous, and not douching can help avoid trichomoniasis.
Overall, trichomoniasis is common but treatable. Recognizing its symptoms early and seeking medical help promptly are crucial. Practicing safe sex is a simple yet effective way to stay healthy and stop the infection from spreading.
FAQ
What is trichomoniasis?
What are the symptoms of trichomoniasis?
How is trichomoniasis treated?
How can trichomoniasis be prevented?
How is trichomoniasis diagnosed?
What are the potential complications of untreated trichomoniasis?
Can trichomoniasis be spread through non-sexual contact?
Can trichomoniasis recur after treatment?
Source Links
- https://www.mayoclinic.org/diseases-conditions/trichomoniasis/symptoms-causes/syc-20378609
- https://www.webmd.com/sexual-conditions/trichomoniasis
- https://www.nhs.uk/conditions/trichomoniasis/
- https://www.cdc.gov/trichomoniasis/about/index.html
- https://www.nhs.uk/conditions/trichomoniasis/diagnosis/
- https://www.testing.com/tests/trichomoniasis-testing/
- https://www.cdc.gov/std/treatment-guidelines/trichomoniasis.htm
- https://www.everlywell.com/blog/sti-testing/untreated-trichomoniasis/
- https://www.who.int/news-room/fact-sheets/detail/trichomoniasis
- https://www.nhs.uk/conditions/trichomoniasis/treatment/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5475227/
- https://www.everlywell.com/blog/sti-testing/trichomoniasis-vs-bv/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8594503/
- https://www.empr.com/home/features/trichomoniasis-management-is-it-reinfection-resistant-infection/2/
- https://www.healthline.com/health/pregnancy/infections-trichomoniasis
- https://www.babycenter.com/pregnancy/health-and-safety/trichomoniasis-during-pregnancy_1427388
- https://www.ncbi.nlm.nih.gov/books/NBK534826/
- http://publichealth.lacounty.gov/dhsp/Trich.htm
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4553853/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7430691/
- https://www.healthline.com/health/how-can-you-get-trichomoniasis-if-no-one-cheats
- https://emedicine.medscape.com/article/230617-overview
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC523559/