Have you ever experienced the feeling of fragility? The sensation that every step you take might shatter the very foundation beneath you? I have. It was a devastating blow to my independence and a wake-up call to the importance of bone health. Osteoporosis, a bone disease that silently weakens and deteriorates our skeletal structure, turned my world upside down.
Osteoporosis is more than just a condition; it’s a thief that steals the strength and vitality from our bones, leaving us vulnerable to fractures and diminished mobility. It affects millions of Americans, particularly women and postmenopausal women, and the impact can be life-altering. But there is hope. By understanding the causes, recognizing the symptoms, and taking proactive steps towards prevention, we can reverse the course of osteoporosis and reclaim our bone health.
In this article, we will delve into the intricacies of osteoporosis, exploring its underlying causes, the importance of bone density, and the lifestyle factors that affect our skeletal well-being. We will uncover targeted exercises, discover the role of supplements, and explore the various treatment options available. By arming ourselves with knowledge and embracing a holistic approach to bone health, we can overcome the challenges posed by osteoporosis and restore strength to our bones, one step at a time.
Key Takeaways:
- Osteoporosis silently weakens and deteriorates bones, making them more prone to fractures
- Understanding the causes and symptoms of osteoporosis is essential for prevention and management
- Bone density plays a vital role in bone health and can be improved through targeted exercises and supplements
- Lifestyle factors, such as diet and physical activity, greatly impact bone health
- Early detection through bone density tests can guide personalized prevention and treatment strategies
Defining Osteoporosis and Its Significance
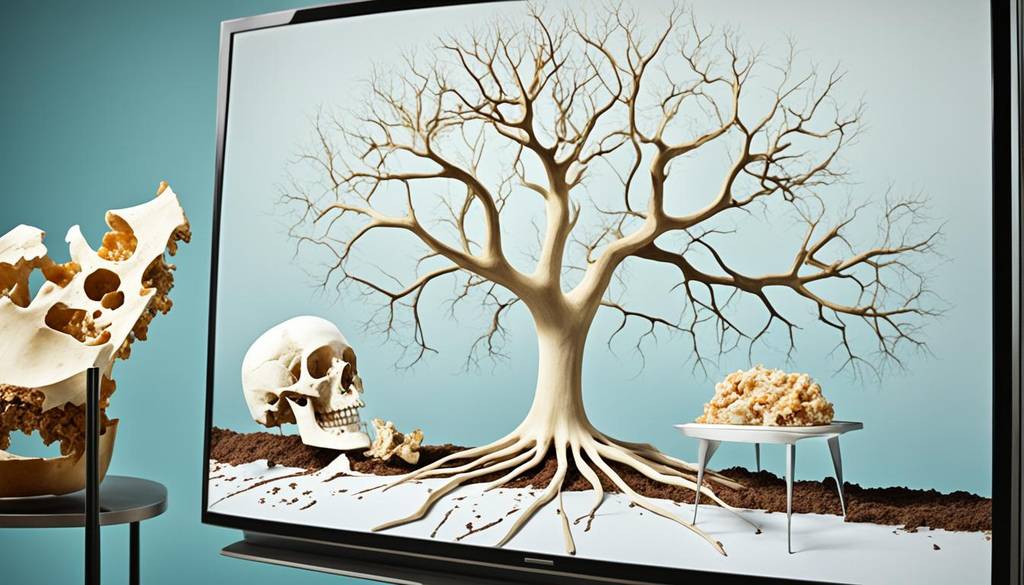
Osteoporosis is a bone disease characterized by the gradual thinning and weakening of bones, making them more susceptible to fractures. It occurs when there is a loss of bone mineral density and mass, resulting in porous and brittle bones.
Osteoporosis is often referred to as a “silent” disease because it typically does not cause any symptoms until a fracture occurs. However, the significance of osteoporosis lies in its impact on overall health. Fractures caused by osteoporosis can lead to chronic pain, loss of mobility, and reduced quality of life. Osteoporotic fractures, especially in the hip, spine, and wrist, can have severe consequences, particularly in older adults.
Osteoporosis is a prevalent condition, affecting approximately 10 million Americans. While it is more common in women, with postmenopausal women being at the highest risk, men can also develop osteoporosis, although at a lower rate. Understanding the definition and significance of osteoporosis is crucial in recognizing the importance of proactive prevention and management strategies.
| Key Points: |
|---|
| Osteoporosis is characterized by the thinning and weakening of bones, making them prone to fractures. |
| It is often referred to as a “silent” disease because it typically does not cause any symptoms until a fracture occurs. |
| Osteoporosis can have a significant impact on overall health, leading to chronic pain, loss of mobility, and reduced quality of life. |
| About 10 million Americans are affected by osteoporosis, with women at a higher risk, especially after menopause. |
Exploring the Anatomy of Bone Density
Bone density plays a vital role in determining the strength and integrity of bones. It refers to the amount of mineral content, particularly calcium, present in the bones. Understanding the anatomy of bone density is essential in comprehending the mechanisms underlying osteoporosis.
Understanding Bone Remodeling
Bone remodeling is a continuous process that occurs throughout life. It involves the removal of old bone tissue (resorption) and the formation of new bone tissue. This dynamic process helps maintain bone strength and structure, ensuring that bones remain healthy and functional. When bone resorption exceeds bone formation, however, bone density decreases, leading to a higher risk of fractures and the development of osteoporosis.
Bone remodeling is regulated by a delicate balance between osteoblasts, cells responsible for bone formation, and osteoclasts, cells responsible for bone resorption. Osteoblasts deposit new bone tissue, while osteoclasts break down existing bone tissue. This constant turnover allows bones to adapt to the stresses placed upon them and repair any microdamage that may occur. The coordination between osteoblasts and osteoclasts is essential for maintaining optimal bone density and preserving bone health.
The Role of Calcium in Bone Health
Calcium is a key mineral for bone health. It provides the structural framework for bones and is involved in various physiological processes within the body. Adequate calcium intake is crucial for maintaining optimal bone density and preventing osteoporosis.
Calcium plays a vital role in bone mineralization, where calcium salts are deposited in the bone matrix, contributing to its strength and density. When blood calcium levels are low, calcium is released from the bones into the bloodstream to maintain the body’s calcium balance. If dietary intake of calcium is insufficient, this constant withdrawal of calcium from the bones can lead to a decrease in bone density over time.
It is recommended that adults consume 1000-1200 milligrams of calcium per day, with higher amounts recommended for individuals at risk for osteoporosis, such as postmenopausal women. Good dietary sources of calcium include dairy products, leafy green vegetables, and fortified foods. In cases where dietary intake is inadequate, calcium supplements may be recommended to ensure optimal bone health.
Understanding the intricate relationship between bone remodeling, calcium, and bone density is essential for the effective prevention and management of osteoporosis. By promoting bone health through adequate calcium intake and supporting the natural bone remodeling process, individuals can maintain strong and healthy bones throughout their lives.
Identifying Osteoporosis Symptoms and Risks
Recognizing the symptoms and understanding the risk factors associated with osteoporosis are crucial for early detection and intervention. Osteoporosis is often considered a “silent” disease because it does not commonly cause symptoms until a fracture occurs. However, there are certain signs that may indicate the presence of osteoporosis, such as back pain, loss of height or stooped posture, and frequent fractures.
Identifying these symptoms can prompt individuals to seek medical attention and receive appropriate diagnosis and treatment. By understanding the risk factors associated with osteoporosis, individuals can determine their likelihood of developing the condition. Age, gender, family history, certain medical conditions, lifestyle factors, and medication use are among the key risk factors for osteoporosis.
By recognizing symptoms and understanding risk factors, individuals can take proactive steps in managing and reducing their risk of osteoporosis, ultimately promoting better bone health and overall well-being.

Osteoporosis: A Silent Epidemic
Osteoporosis has been aptly termed a “silent” epidemic, as it often goes undetected until a fracture occurs. The lack of visible symptoms and awareness surrounding the condition contributes to its underdiagnosis and increasing prevalence worldwide. Individuals may not seek medical attention until they experience a fracture or significant bone loss, leading to delayed intervention.
Undetected osteoporosis can have severe consequences, including chronic pain, disability, reduced mobility, and increased mortality. The economic burden of managing osteoporotic fractures is also substantial. It is essential to raise awareness about this silent epidemic, promote early detection strategies, and encourage proactive prevention measures to address this significant public health issue.
Why Osteoporosis is Often Undetected
The asymptomatic nature of osteoporosis is the primary reason behind its frequent underdetection. The absence of visible symptoms makes it challenging for individuals to recognize the condition and seek medical attention. As a result, osteoporosis often goes undiagnosed until a fracture occurs or significant bone loss is detected.
The Consequences of Undiagnosed Osteoporosis
Undiagnosed osteoporosis can have severe consequences for individuals. Fractures resulting from weakened bones can cause chronic pain, disability, and reduced mobility. The impact of these fractures on daily life and overall well-being is significant. Additionally, undiagnosed osteoporosis can increase the risk of mortality, especially in older adults. The economic burden of managing fractures and their long-term consequences places a substantial strain on healthcare systems and the economy as a whole.
It is crucial to prioritize early detection, raise awareness about osteoporosis, and encourage individuals to undergo bone density testing to identify the condition in its early stages. By doing so, appropriate intervention and management strategies can be implemented to mitigate the consequences of undiagnosed osteoporosis.

The Causes of Bone Density Deterioration
Bone density deterioration is a key factor in the development of osteoporosis. Understanding the underlying causes of this deterioration is essential in effectively managing the condition.
Several factors contribute to bone density deterioration:
- Aging: As people age, bone remodeling becomes less efficient, leading to a gradual loss of bone density.
- Hormonal Changes: Hormonal changes, such as the decline in estrogen levels during menopause for women, can accelerate bone loss.
- Lifestyle Factors: Poor nutrition, sedentary behavior, smoking, and excessive alcohol consumption can also contribute to bone density deterioration.
- Medication Use: Certain medications, such as corticosteroids, anticonvulsants, and cancer treatments, can negatively impact bone health.
- Medical Conditions: Certain medical conditions, such as endocrine disorders and gastrointestinal diseases, can increase the risk of bone density deterioration.
Identifying and addressing these underlying causes are crucial in preventing and managing osteoporosis effectively.
Addressing the Gender Disparity in Osteoporosis
Osteoporosis is a bone disease that affects both men and women, but there is a gender disparity in its prevalence and impact. Women are at a higher risk of developing osteoporosis compared to men, primarily due to factors such as hormonal changes during menopause and lower peak bone mass.
Osteoporosis in Women: A Closer Look
In women, osteoporosis is closely associated with postmenopausal osteoporosis, which occurs due to the decline in estrogen levels. Estrogen plays a crucial role in bone health, and the decrease in its production during menopause can lead to bone loss and increased susceptibility to fractures. Women also have lower peak bone mass compared to men, making them more vulnerable to the effects of bone density deterioration.
Understanding the specific risk factors and management strategies for osteoporosis in women is essential in addressing their unique needs. Proactive measures such as adequate calcium and vitamin D intake, weight-bearing exercises, and regular bone density testing can help women maintain optimal bone health and reduce the risk of fractures.
Understanding Osteoporosis in Men
Osteoporosis in men is often underdiagnosed and undertreated, as it is more commonly associated with women. However, men can also experience bone loss and fractures as they age. Although men have a higher peak bone mass and a slower rate of bone loss compared to women, other factors such as hormonal imbalances, certain medical conditions, and medication use can contribute to osteoporosis development.
Understanding the risk factors, symptoms, and management approaches for osteoporosis in men is crucial in promoting early detection and effective treatment. Men should be aware of the importance of maintaining bone health through a balanced diet, regular exercise, and routine bone density testing. By addressing the specific needs and challenges associated with osteoporosis in men, healthcare professionals can help prevent complications and improve the overall well-being of male patients.

Lifestyle Factors Affecting Osteoporosis
Lifestyle factors play a significant role in the development and management of osteoporosis. Two key factors that influence bone health are diet and physical activity.
The Influence of Diet and Nutrition
Proper nutrition is essential for maintaining optimal bone density and preventing osteoporosis. Incorporating calcium-rich foods into your diet is crucial, as calcium is a key mineral for bone health. Sources of calcium include dairy products, green vegetables, and calcium-fortified products. It is also important to ensure adequate intake of vitamin D, as it helps with calcium absorption. Vitamin D can be obtained through sunlight exposure and supplementation if necessary.

The Impact of Physical Activity on Bone Health
Physical activity is another crucial lifestyle factor that affects bone health and helps prevent bone density deterioration. Engaging in weight-bearing exercises is especially beneficial for promoting bone strength. Activities such as walking, jogging, dancing, and hiking put stress on the bones and stimulate bone formation. Additionally, muscle-strengthening exercises and balance exercises can improve overall physical function and reduce the risk of falls and fractures.
By understanding the influence of diet, nutrition, and physical activity on bone health, individuals can make informed lifestyle choices to prevent and manage osteoporosis effectively.
Targeted Exercises for Osteoporosis Management
Targeted exercises are an essential component of managing osteoporosis. By incorporating specific exercises into your routine, you can improve bone density, strength, and reduce the risk of falls and fractures. Two types of exercises that are particularly beneficial for bone health are weight-bearing exercises and non-impact exercises.
Weight-Bearing Exercises for Osteoporosis
Weight-bearing exercises involve activities that put stress on the bones, promoting bone formation and improving bone density and strength. These exercises are important for managing osteoporosis effectively. Some examples of weight-bearing exercises for osteoporosis include:
- Walking
- Jogging
- Dancing
- Hiking
Engaging in these weight-bearing exercises on a regular basis can help strengthen your bones and reduce the risk of fractures. They are simple, low-cost, and can be easily incorporated into your daily routine.
Non-Impact Exercises: A Complementary Approach
In addition to weight-bearing exercises, non-impact exercises provide a complementary approach to managing osteoporosis. These exercises focus on improving balance, flexibility, and muscle strength, reducing the risk of falls and fractures. Some examples of non-impact exercises for osteoporosis include:
- Tai Chi
- Yoga
- Swimming
- Cycling
Non-impact exercises are gentle on the joints and are particularly beneficial for individuals who may have limitations or prefer low-impact activities. Incorporating a combination of weight-bearing and non-impact exercises into your routine can help you effectively manage osteoporosis and reduce the risk of complications.
The Role of Supplements in Osteoporosis Prevention
Supplements can play a supportive role in osteoporosis prevention by providing additional nutrients that are crucial for bone health. Calcium and vitamin D are the two main supplements associated with osteoporosis prevention.
Calcium supplements can help individuals meet their daily calcium requirements when dietary intake is insufficient. Adequate calcium intake is crucial for maintaining optimal bone density and preventing osteoporosis.
Vitamin D supplements, particularly for individuals who have limited sunlight exposure or have difficulty absorbing vitamin D from food sources, can help enhance calcium absorption and support bone health. Vitamin D is essential for proper calcium absorption and utilization in the body.
Other supplements, such as magnesium, vitamin K, and omega-3 fatty acids, may also have potential benefits for bone health. Magnesium is involved in bone formation and metabolism, vitamin K helps regulate calcium in the body, and omega-3 fatty acids have anti-inflammatory effects that can support overall bone health.
However, it is important to consult with healthcare professionals before starting any supplements, as individual needs may vary based on factors such as age, gender, and underlying health conditions. Healthcare professionals can provide personalized recommendations and dosage guidelines based on specific needs and potential interactions with medications or medical conditions.
By incorporating appropriate supplements into a comprehensive osteoporosis prevention plan, individuals can enhance their bone health and reduce the risk of developing osteoporosis. It is essential to remember that supplements should not replace a balanced diet or a healthy lifestyle. They should be used as a complementary approach to support overall bone health and preventive measures for osteoporosis.
Osteoporosis Treatment Options
Bisphosphonates and Their Effectiveness
Osteoporosis, a condition characterized by low bone density and increased risk of fractures, can be effectively managed and treated through various medical interventions. One commonly prescribed class of medications for osteoporosis is bisphosphonates. Bisphosphonates work by inhibiting bone breakdown and promoting bone formation, thereby reducing the risk of fractures and improving bone density.
Studies have shown that bisphosphonates are highly effective in treating osteoporosis. They have been found to increase bone mineral density and reduce the incidence of fractures, particularly in postmenopausal women. These medications work by slowing down the activity of cells that break down bone tissue, known as osteoclasts. By inhibiting bone resorption, bisphosphonates help maintain or increase bone density, making them an essential component of osteoporosis treatment.
Commonly prescribed bisphosphonates include alendronate (Fosamax), risedronate (Actonel), and ibandronate (Boniva). These medications are usually taken orally on a weekly or monthly basis, depending on the specific drug and dosage prescribed. In some cases, intravenous bisphosphonates, such as zoledronic acid (Reclast), may be administered annually.
Emerging Therapies in Bone Density Management
In addition to bisphosphonates, there are emerging therapies in bone density management that show promise in improving bone health and preventing fractures. These innovative treatments aim to target specific pathways involved in bone metabolism and provide alternative options for individuals who may not respond well to or tolerate bisphosphonates.
One emerging therapy is the use of monoclonal antibodies, such as romosozumab (Evenity) and denosumab (Prolia). These medications work by inhibiting a protein called sclerostin, which plays a role in bone breakdown. By blocking sclerostin, these medications help promote bone formation and increase bone density.
Another promising therapy is the use of newer pharmacological agents, such as abaloparatide (Tymlos) and teriparatide (Forteo). These medications work by stimulating bone formation and can be used in individuals at high risk of fractures or those who have failed other treatments.
It is important to note that the choice of treatment for osteoporosis depends on various factors, including the severity of the condition, medical history, and individual needs. Consulting with healthcare professionals is crucial in determining the most appropriate treatment options to effectively manage osteoporosis and reduce the risk of fractures.
Understanding and Obtaining a Bone Density Test
Bone density tests are diagnostic tools used to assess bone health and diagnose osteoporosis. Understanding when and why to consider a bone density test is crucial for early detection and intervention.
When and Why to Consider a Bone Density Test
Certain factors, such as age, gender, medical history, and risk factors for osteoporosis, may indicate the need for a bone density test. Women over the age of 65 and men over the age of 70 are generally recommended to undergo a bone density test. Additionally, individuals with specific risk factors or medical conditions that can affect bone health may also benefit from a bone density test.
By evaluating bone density, the test can identify if an individual has osteoporosis or if their bones are at risk of fracture. Early detection allows for timely interventions to prevent further bone loss and reduce the risk of fractures.
The Procedure of a Bone Density Test
The procedure of a bone density test typically involves a painless and noninvasive scan that measures the mineral density of bones. The most commonly used technique for bone density testing is dual-energy X-ray absorptiometry (DXA). During the test, the patient lies on a padded table while a machine scans specific bones, such as the hip and spine, to determine their density.
The results of the test are usually presented as a T-score, which compares the patient’s bone density to that of a healthy young adult. A T-score of -1.0 or above is considered normal, while a T-score between -1.0 and -2.5 indicates low bone mass (osteopenia), and a T-score of -2.5 or below indicates osteoporosis.
Conclusion
Osteoporosis is a prevalent bone disease that can have severe consequences if left undiagnosed and untreated. Understanding the causes of osteoporosis, its symptoms, and risks is crucial for early detection and intervention. Bone density deterioration, gender disparities, and lifestyle factors also play significant roles in the development and management of osteoporosis. Targeted exercises, proper nutrition, and the use of supplements can help improve bone health and prevent further bone density loss.
Early detection of osteoporosis through bone density testing is essential for timely intervention. Lifestyle modifications, such as regular physical activity and adherence to prescribed medications, can reduce the risk of fractures and improve overall bone health. It is crucial for individuals to prioritize their bone health and seek medical guidance for personalized prevention and management strategies.
By taking proactive measures, individuals can maintain strong and healthy bones throughout their lives and reduce the impact of osteoporosis. Remember, prevention is key. By understanding the symptoms, risks, and management options for osteoporosis, individuals can lead an active and fulfilling life while safeguarding their bone health.
FAQ
What is osteoporosis?
How common is osteoporosis?
Who is at a higher risk of developing osteoporosis?
What are the symptoms of osteoporosis?
What causes bone density deterioration?
Why is there a gender disparity in osteoporosis?
How can lifestyle factors affect osteoporosis?
What are targeted exercises for osteoporosis management?
How can supplements help in osteoporosis prevention?
What are the treatment options for osteoporosis?
When should I consider a bone density test?
What is the procedure of a bone density test?
Source Links
- https://www.niams.nih.gov/health-topics/osteoporosis
- https://www.mayoclinic.org/diseases-conditions/osteoporosis/symptoms-causes/syc-20351968
- https://www.webmd.com/osteoporosis/understanding-osteoporosis-basics




